Proposition: Impact for the introduction and implementation of risk stratification for population health management in The Netherlands.
Validation, implementation and extension of the ACG© tool for population management and risk stratification for Dutch (Primary) Health Care Regions
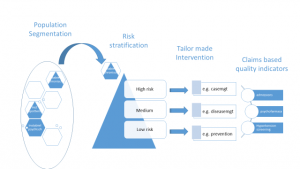
Population health management (PHM) is more and more accepted as a means to support the transition in health care from institutional based to person-centred care. This creates the incentive to move away from the volumebased approach of the institutions to a valuebased approach for the subpopulations. PHM is ideally a datadriven approach which relies heavily on population data-analyses. For PHM three major analyses are needed: population segmentation, risk stratification and outcome assessment.
- Population segmentation: in this endeavour the population is analysed using data from various sources and registries. Through thorough analysis using scenario planning including existing demographic and epidemiologic projection techniques, the current and future main burning platforms in the population have to be
- Risk Stratification: is a systematic process that divides a population into different strata of risk for a specified outcome, e.g. unscheduled admission to hospital or high cost patients. The next step is Case finding for risk stratification which is a systematic process to identify sectors of the population that may benefit from additional clinical intervention, as directed by a lead clinician such as the patient’s GP. This analysis can be carried out on data sources of various health care providers (hospital, primary care etc)
- Outcome assessment: PHM aims at improving health, patient experience and lower cost per capita. To assess whether this datadriven approach yields these aims, outcome indicators are needed that are accepted by various stake holders (payers, providers and patients). It is important that these outcome indicators are SMART formulated and feasible to measure and monitor. In this proposal claims based quality indicators will be developed.
The approach is illustrated as follows:
 In the current transition towards more integrated regional health networks, several initiatives are developing integrated data infrastructures. Examples like Nijkerk, ‘Gezonde Zorg, Gezonde Regio’ and the activities of VIP Calculus/Proïgia show the ambition and necessity, and at the same time the struggle, to combine data from various data sources like primary care, pharmacy, hospital and other claims data. First attempts are being made to include home care and social care data.
In the current transition towards more integrated regional health networks, several initiatives are developing integrated data infrastructures. Examples like Nijkerk, ‘Gezonde Zorg, Gezonde Regio’ and the activities of VIP Calculus/Proïgia show the ambition and necessity, and at the same time the struggle, to combine data from various data sources like primary care, pharmacy, hospital and other claims data. First attempts are being made to include home care and social care data.
The second part of the ambition is to find the right information and tooling to seduce the professionals and organisations to change their behaviour. Appropriate Business Intelligence tooling for this purpose is in development in The Netherlands.
The Jan van Es Institute, in collaboration with Raedelijn, has performed a literature review on the existing methods that support PHM activities like population segmentation, risk stratification and outcome measurement. This review resulted that the ACG-method outperformed the other five methods.
The ACG system is developed by Johns Hopkins Institute in Baltimore and relies on more than 30 years of research. It is widely used in various parts of the world.
In the Netherlands GPs in several regions (Urk, Nijkerk, Zoetermeer, Haagse Schilderswijk en Wassenaar) have shown their interest in using the ACG system to gain more insight in their target populations. By using the ACG system they expect that they will implement more tailored interventions according to the specific needs of their population.
The aim of this proposal is to assess the usability of the ACG system, in terms of validity, reliability, practicality and impact of specific aspects of a PHM approach (population segmentation and risk stratification followed by tailor-made interventions) in (primary) care settings.
Subsequently the validation, the spread of the classification is accompanied by various activities with the aim that in 2020 50% of all primary care groups make use of this specific tooling.
Work plan
To fulfil the aims of this proposal we distinguish between two phases. During the first phase of 18 months we perform two main activities:
- the analyses to validate and calibrate the ACG system in 5 different GP regions
- the preparation of the implementation of the system in Dutch (primary) health care
During the second phase we aim at realising the spread/implementation of the system. The current proposal is for the first phase of 18 months.
Validation and Research
Patients and Practices
This proposal will be carried out in collaboration with five groups of general practices in different areas in The Netherlands: a regional health care initiative op Urk (20.000 inhabitants), two health care centers in Nijkerk (appr. 30.000 inhabitants), all general practices in Zoetermeer (appr 110.000 inhabitants), 8 general practices in de Haagse Schilderswijk (appr 40.000 inhabitants) and all general practices in Wassenaar (26.000 inhabitants). Zilveren Kruis and CZ as major health insurers in these areas will be invited to participate in this proposal. Using the claims data from the insurance companies the impact on secondary and tertiary care can be assessed.
During this phase the validation of the ACG system and the assessment of the claims based quality indicators are central.
- Validation of the ACG system.
The ACG system and its algorithms are based on US and UK data and need to be validated for the Dutch situation with Dutch data. In a previous study, JVEI performed first analyses on the GP data of Nijkerk. The result was that Dutch GP data were very well structured (ICPC for diagnoses and ATC for medication) and could be processed easily in the ACG software. The results of these analyses were well appreciated by the care providers.
Casemix has applied the ACG classification on the data from the Lange Land Ziekenhuis and showed the potential for risk stratification in hospitals. In a next step the system was applied on the data from three hospitals in analysing the risk profile of the subpopulation of Orthopedic patients.
After the technical feasibility, the validity of the system needs to be assessed. We distinguish three levels : .
- Face validity. Based on a random sample of 20 patients per general practice, the classification of each person into one or more EDC and ADG categories, the labelling of a major ADG and the final placement in one ACG category will be verified by the GP. We assess the number of patients that are categorised correctly according to the GP.
- Convergent validity. Based on the comparison between specific indicators for the total population as computed by the ACG algorithms with indicators based on other categorisations. For example, the chronic conditions count in the ACG should correlate highly with the number of chronic conditions as registered by the GP on his problem list. Comparisons of around 50% of the patients will be carried out.
- Predictive validity. We assess to what extent the predictive values generated by the ACG system using the GP data correspond with the registered data in the claims database including hospital costs. The predictions that are considered are for hospital admissions (6 and 12 months), emergency care visits, unexpected medication use, total health care costs and persistent high user of care. The analyses will be carried out GP data for 2014 and 2015 and registered claims data for 2015 and 2016. Based on these analyses, the algorithms will be calibrated for the Dutch GP situation. Since we have five different areas we can adjust the algorithms in specific areas and validate the new adjusted algorithms in other areas. By using the claimsdata the validity of the prediction of hospital admissions and hospital costs can be assessed.
Implementation in pilot regions (5 GP areas)
To assess the practicality of the ACG tool we perform the analysis in 5 different areas on 2017 data. The current output of the ACG system is not tailored for Dutch primary health care. To make it applicable for Dutch primary care, a specific set of reports needs to be developed. To illustrate the potential of the ACG approach a set of infographics will be produced showing (1) the relevant population segmentation in terms of ACG categories in combination with relevant information as major ADG count, chronic condition count, health care use, age, gender and neighbourhood (derived from ZIP code), (2) the risk stratification in the various segments as expressed by the various predictions on adverse outcomes (hospital admissions, emergency care visits, high costs etc) and (3) selected claims based quality indicators, as prioritised through the Delphi method. These infographics will be produced from a database which can be used for more in-depth analysis in subsequent sessions with the involved practices.
The reporting tool is accompanied by training sessions with the primary care providers and their supporting staff to recognise their population and further interpret the potential of the new acquired information.. These sessions will take place both local as central with all groups together in order to stimulate the mutual knowledge exchange. A network of ‘first movers’ is thus created.
The output for the participating GP-areas is an extended report of their population for 2017 (next to the reports made for 2014-2016 to assess the validity of the system), accompanied by first ideas about the Triple Aim interventions that could be implemented.
Together with health care professionals and their supporting staff of the 5 GP areas, the standard report and the training sessions are developed. The input of the end-user (GP professional and supporting staff) is crucial for the acceptance of the concluding report and the start of the dissemination by the concept by training all providers in The Netherlands.
Subsequently, the report gives direction for the interventions that could be carried out in the target population.
The practicality of this approach is assessed by
- Whether the health care providers develop and implement interventions based on the outcomes of the risk analyses.
- Whether the health care providers experience the ACG classification as a valuable tool to assess the burden of disease of their population and reports as valuable for the management of the health of their population..
- Whether the health insurers are willing to accept this classification as a tool to describe the needs of this population and to give financial support to interventions to improve the health of the population. (e.g. using the new O&I possibilities).


